'A Breakdown In Communication:' SoonerSelect Managed Care Program Meets Mixed Reviews
SoonerSelect launched just over a week ago, and the response is mixed. The program changes the way Medicaid is administered through SoonerCare.Tuesday, April 9th 2024, 5:47 pm
OKLAHOMA CITY, Okla. -
SoonerSelect launched just over a week ago, and the response is mixed.
The program changes the way Medicaid is administered through SoonerCare. SoonerSelect is a managed care program, meaning members must now choose one of three contracted plans.
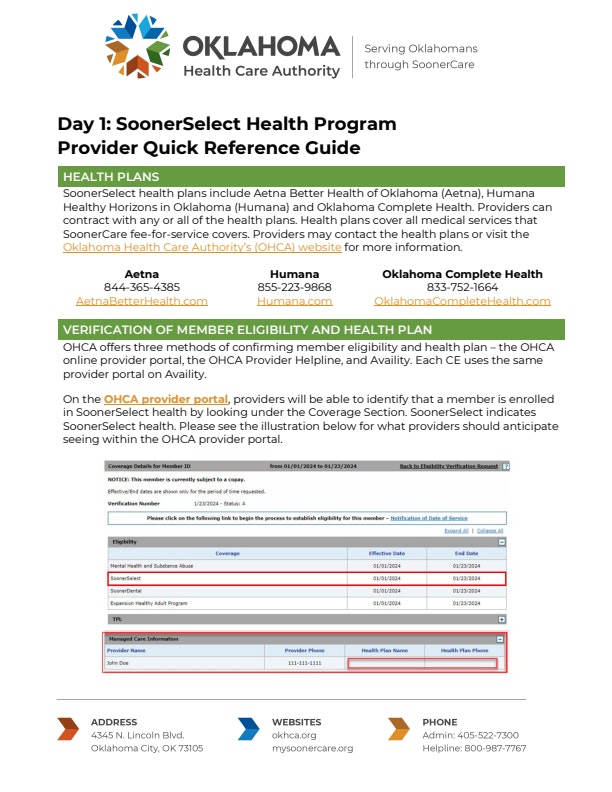
Those companies are Aetna BetterHealth, Humana Healthy Horizons of Oklahoma, and Oklahoma Complete Health.
This means providers submit insurance claims to these third-party companies and no longer collect reimbursement for SoonerCare clients directly from the state. Some healthcare providers say the transition has been a nightmare, while others say they're not seeing any issues. Most of the concerns are coming from smaller, independent healthcare practices who say there's a communication breakdown. "I feel like it can work if it's rolled out correctly," Shay Espinosa, a licensed professional counselor at Integrated Therapy Solutions, said.
"We've all been told as providers everything will be the same," she said. “Pay will be the same, pay codes will be the same, we just have to run them through these managed care companies, and that's not what we're experiencing at all."
Espinosa says small providers across the state are having the same issues. "For our providers, they're all service fees, so they don't get paid until the claims get paid," she explained.
She went on to say that no payments have been made. "Our agency alone has submitted over a thousand claims, and we've received 53 that are pending," Espinosa said.
"Moving to managed care in our state is a very major shift," Variety Care CEO Lou Carmichael said.
She added her Oklahoma community health center has experienced a smooth transition to SoonerSelect. "I think there's a lot of confusion but we're moving over three million people to a new way of doing things," she said.
Before the launch, the OHCA's website provided training guides and info sheets for providers.
The help sheet for providers can be found here:
"I think the healthcare authority has done a really great job of navigating this with so much changing at once," Carmichael said.
"We're a smaller scale," Espinosa said, adding the lack of administrative infrastructure is what's making the transition hard on smaller providers. “It's a breakdown in communication. I think these three contracted entities were not given the correct information."
Espinosa fears it may create a bigger disparity for Medicaid recipients. "Providers are already leaving Medicaid,” she said. “They already started referring their clients out at the end of last week and said, ‘I'm done, I’m not messing with it.’"
News 9 spoke with representatives at the Oklahoma Healthcare Authority who maintain they're here to help. Chief of Staff Christina Foss said one plan reports 40,000 claims will be paid out today and Thursday.
She is encouraging all members and providers to reach out with concerns. "If a provider has a question or they feel like they're not getting the proper response from a plan, reach out to us,” Foss said. “That's our job as an agency is to hold these plans accountable.”
So, what's the best way for people to voice these concerns with the healthcare authority? If you have concerns as a member, you can call 800-987-7767 or email soonerselect@ohca.org.
Providers are also encouraged to use that email and utilize the resources on the OHCA website.
Cameron Joiner
Cameron Joiner joined the News 9 team as a Multimedia Journalist in January of 2023. Cameron was born and raised in Sugar Land, Texas, just outside of Houston. Though she is a Texan at heart she has fallen in love with Oklahoma. She came to the Sooner State to attend OU, where she majored in Broadcast Journalism.
More Like This
April 9th, 2024
December 26th, 2024
December 26th, 2024
December 26th, 2024
Top Headlines
December 26th, 2024
December 26th, 2024
December 26th, 2024
December 26th, 2024